Grounded in understanding my chronic condition
Anna is a student researcher at Tufts University, an aspiring physician, and an adult living with primary immunodeficiency. In this blog, Anna shares with Rebekah what has grounded her as she navigates life with a recent diagnosis of her specific mutation.
R: What is unique about managing primary immunodeficiency?
A: I recognize that PI is an incredibly diverse group of conditions, and my treatments might not necessarily translate to other conditions. For the longest time, my body wasn’t producing red blood cells. It wasn’t until I transitioned to a different immunologist when I became an adult that I got the genetic testing done and found out about my specific mutation. I was initially diagnosed with CVID when I was 12 years old, but I’ve recently been recategorized with STAT3 gain-of-function (GOF) mutation after genetic testing. I was actually surprised to hear my specific mutation mentioned at least 5 times during the IDF conference because it only affects around a hundred people in the world that we know of.
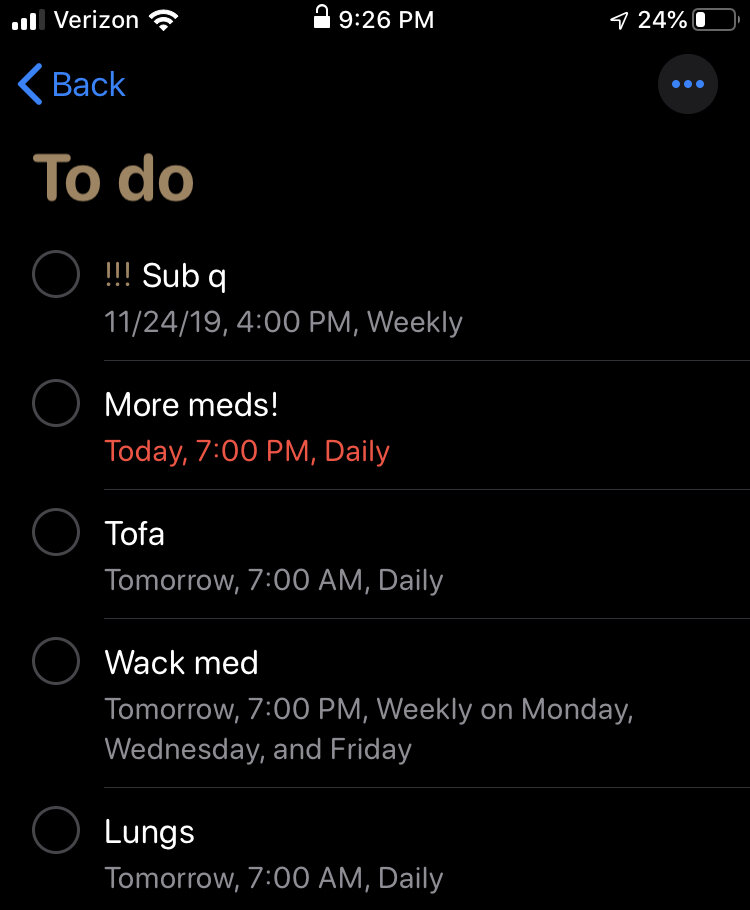
This means that my new diagnosis came as I transitioned to adulthood. And there’s a lot to keep track of. The medications that I take on Mondays, Wednesdays, Fridays are particularly difficult to remember. I receive reminders on Folia so that I remember to do the treatments and click “all done” or “some done” in the app. I find it helpful to match an event to certain treatments, so I do my lung therapy before getting dressed in the morning.
Although this new diagnosis has been difficult to navigate, I have the support of my family and friends. I was also lucky in that there were already existing treatment that targets the specific pathway for this mutation.
“I wish I had written down all of my symptoms when I first switched medications ”
A screenshot of Anna’s reminders pre-Folia
I wish I had written down all of my symptoms when I first switched medications because it was crazy. I’ve always struggled with chronic fatigue, eczema, GI issues, hematological issues… I switched medications last February, and within a couple of weeks, I could see drastic improvements. I ran up to my doctor and told her “look at my hands!”. I used to have really dry hands as one of the symptoms, but now my hands look pretty nice!
R: How has your interest in science and role as a student researcher influenced the way you approach your condition?
A: I’m definitely a touch eccentric in my interest in science, but I’ve found it very grounding to understand my condition. So despite how frustrating it is, having some scientific background to be able to understand why my body reacts in the way it does is actually really helpful.
For the PI community right now, we’re starting to understand the genetics of the immune system more and more, so a lot of CVID patients are getting their genetic diagnosis, and that sheds a lot of light onto the subject. It helps to understand yourself a little more.
I've also been surprised to learn how medical researchers actually lack data on the everyday symptoms people experience when managing chronic conditions. During the literature review in my Darwinian medicine class, I realized that the data I would need for my project on multiple sclerosis (MS) were not available! The journal articles didn’t trace the findings to the specific types of MS. Having an insight into different symptoms based on the specific types of condition is something that I would so desperately want for studying MS. With an app like Folia, you can constantly track your observations, so there’s so much more that you can understand.
R: How has your interest in medicine impacted how you communicate with your care team?
A: My dad’s role as a family doctor has been one of the driving forces for me to go into medicine. As we’re both science-oriented, my dad has been a great educator. He would read the literature on my condition, and now it’s me reading the literature.
When you have an interest in medicine, I think the relationship with your doctor changes a lot. I have a cute story - I had a lung biopsy last year, and when the anesthesiologist found out that I was premed, he brightened up and explained the epidural by drawing a schematic. It’s unfortunate that a lot of people don’t have a chance to see that because doctors don’t have much time to explain every little detail, but having an intellectual and patient-based relationship with your care team is pretty cool.
Anna skydiving!
R: Tell us about your interest in the outdoors and adventure!
A: I love exploring, skiing, swimming, and overall adventuring. My parents are very into exercise, so they’ve always pushed me to share a similar passion for it. It also helps that exercise/being outdoors in general is fantastic for my lungs.